Dental Implants

Dental implants are the standard of care for the replacement of missing teeth. The process of placing and restoring dental implants generally takes six months to a year. Total time necessary for treatment depends on the number of implants, location, and how the implants are being restored.
Surgeon Evaluation
Dental Implants are surgically placed directly into your jawbone by a dental specialist with extensive training in implant placement and complications that may arise. Not every patient is a good candidate for dental implants. We will recommend that our patients receive a surgical evaluation prior to finalization of an implant treatment plan.
Diagnostic models and X-rays are required for all implant candidates. Many patient models will also be discussed with our dental implant lab partners prior to final treatment plan presentation. After your visit with the surgeon and our discussion with the lab, a final treatment plan including anticipated time frame and fees will be presented. It is important to keep in mind that the surgeon's fees for implant placement and our fees for treatment received at Steckelberg Dental are separate fees.
Healing Stages
After dental implant placement, you will undergo a healing phase. During this time your body is building bone around the implant, called osseointegration. We must wait until the implant is stable in your bone before we place forces on the implant. The surgeon who places the implant will let us know when it is time to restore your implant.
Sometimes a second stage surgery is required. This is often done to uncover implants placed deep in your gum tissue. Implant placement is dictated by the amount of bone available. Thus, your implant surgeon makes the decision of implant placement location and number of implants placed. Dr. Steckelberg prefers to work with implant surgeons who have received additional training in implant placement and are committed to communication with our office.
Fixture Level Impression or Digital Impressions
In order to have your implant crown or implant denture fabricated in the lab, we utilize a fixture level impression or digital impressions. For the fixture level impression, we temporarily remove your implant's healing cap. A special attachment called an impression coping is secured into your implant. An X-ray must be taken to verify proper fit of the coping prior to your impression. We then take an impression and replace the healing cap. When feasible, we will coordinate a digital impression at your surgeon's office; this will occur during one of the osseointegration check appointments at your implant surgeon's office. We strive for this to appear effortless, but it only happens because of the excellent communication between your implant surgeon's office and our office.
Delivery
The final and most rewarding step of implant treatment is the delivery of your final restoration. It is very common to use a semi-permanent or temporary cement to secure your final implant crown or bridge to your dental implant. This will allow future access to your restoration for maintenance and treatment of any possible future problems.
Periodontal Disease Treatment

Periodontal disease is a term that encompasses a wide variety of dental problems. It may or may not have symptoms that have been visible to you. Bleeding gums, mobile teeth, and bad breath do not always show up early in the disease process. That is why it is important to see a dental professional regularly for screening of periodontal disease and treatment.
Periodontal disease is not treated in one visit. After evaluation and diagnosis of periodontal or "gum disease," your individual treatment needs are presented. Usually, a deep cleaning called "scaling and root planing" is the first step of treatment. If the disease is quite advanced, you may be referred to a periodontist for treatment that may include gum surgery.
Periodontal disease left untreated may result in pain, infection, and tooth loss. Another aspect of periodontal disease to be aware of is the link to systemic diseases. Emerging, new studies continue to tell us more about the link periodontal disease has with your overall health, including cardiovascular disease.
Periodontal disease is characterized by bone loss, inflammation, and quite often dental calculus. Calculus is a hardened material that can only be removed by a dental professional. Over time, leftover foodstuff hardens or calcifies around and below the gum line; we call that calculus or tartar. You can reduce the general amount of tartar present in your mouth with proper daily brushing, flossing and dental mouth rinses. Calculus present under the gum line cannot be removed by brushing harder. It must be removed by a special dental cleaning called scaling and root planing.
Scaling & Root Planing
When active periodontal disease is present, a special deep cleaning, called "scaling and root planing," will be presented as a part of your treatment plan. Scaling and Root Planing is performed under local anesthesia. This is an extension of a regular dental cleaning, called a prophylaxis. The pockets below your gum line are cleaned and rough tooth structure is smoothed. This cleaning helps to reduce the bacteria, inflammation and calculus present in those pockets.
Many patients will be put on a special prescription mouthwash to help reduce bacterial levels. We also may recommend additional dental cleaning aids, such as a proxybrush or electric toothbrush. Ask us about purchasing these products with our in-office discount.
Periodontal Maintenance
After active periodontal disease is treated, you will need to see your dentist on a regular basis for Periodontal Maintenance appointments. At these appointments, we check your pocket measurements and disease status. Periodontal maintenance allows us to clean in the areas that your toothbrush, proxybrush, and mouth rinse cannot reach: in the pockets under your gums. Proper, continued maintenance is the key to winning the battle against gum disease.
Areas of active disease are treated with cleaning and any necessary adjunctive therapy. Some cases may require direct antibiotic placement into the residual pockets. Dr. Steckelberg will let you know if this is appropriate treatment for you. If necessary, this will be done in-office at your periodontal maintenance appointments.
Gum areas that appear stable are also cleaned and monitored at these frequent visits. Periodontal disease can deteriorate quickly if not routinely monitored and treated. Generally speaking, most patients are seen at least four times yearly for this special cleaning. If the disease remains inactive for several visits, then we will let you know if we can see you three times yearly. Our goal is to avoid additional bone loss and repeated scaling and root planing treatments. Most patients with periodontal disease will need to have dental cleanings 3-4 times yearly, instead of the traditional twice yearly schedule.
Crowns and Bridges
Crowns
Having a crown made requires several steps, and generally two dental visits. Your tooth is prepared by removing the outer portion to accommodate the space needed for the crown. After your tooth is prepared, an impression is taken to reproduce an exact model. This model and the impression are sent to the dental laboratory, where your crown is fabricated. In our office, we make a temporary crown to cover your tooth while your permanent crown is made at the laboratory. When it is ready, we cement your new crown in place.
A crown covers a prepared tooth to restore it to the natural shape, size and function. It can strengthen a tooth that has had a large amount of dental decay and a large dental filling. A crown may be needed in the following situations:
- after root canal therapy (endodontic treatment)
- to restore a fractured tooth
- to protect a weak tooth from breaking
- to restore a dental implant
- to cover a discolored or poorly shaped root
Bridges
A bridge is similar to a crown in preparation and steps. Let's talk about a three-unit bridge, which generally replaces one missing tooth. For a three-unit bridge, a crown is made on each side of the missing tooth. A pontic covers up the missing space and attaches those two crowns together. A pontic is made of the same material as the crowns but attaches only to the neighboring teeth.
Having a bridge made requires several steps, and generally two to three dental visits. Your teeth are prepared by removing the outer portion to accommodate the space needed for the crowns. After your teeth are prepared, impressions are taken to reproduce an exact model. This model and the impression are sent to the dental laboratory, where your bridge is fabricated. In our office, we make a temporary crown to cover your tooth while your permanent crown is made at the laboratory. A second appointment, called a try-in, allows us to make any necessary adjustments to the metal framework or "backbone" of your bridge. Not all dental bridges will require the try-in appointment, but if utilized it will be followed by the third cementation appointment. Once you and Dr. Steckelberg are satisfied, your bridge is cemented in place.
If you have had several dental implants placed, a bridge may also be placed over the implants. The steps are similar to having a traditional bridge made, except that most preparation is done outside the mouth. Implants also require additional healing time after surgical placement.
Partial and Complete Dentures
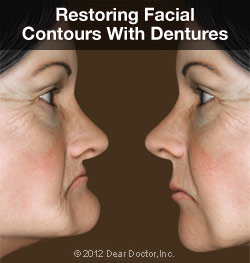
Full or partial tooth loss, if left untreated, doesn't just affect a person's self-image — it can also increase the risk of developing nutritional problems and other systemic health disorders. Fortunately, there's a reliable and time-tested method for treating this condition: full or partial dentures.
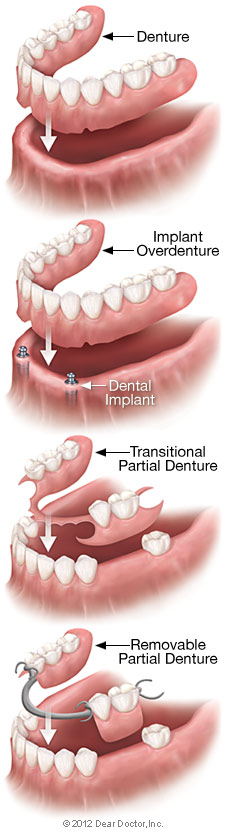
Dentures are just one option for replacing missing teeth; some of the others include fixed bridgework and dental implants. Each method has its particular pluses and minuses, which should be carefully considered. There are also several varieties of dentures available to address specific issues, from partial dentures to implant-supported overdentures. During a consultation, we can explain the available options and help determine which is best in your individual situation.
How Do Removable Dentures Work?
Full or partial dentures consist of a gum-colored base made of plastic resin, which fits over the remaining alveolar (bone) ridge that formerly held the teeth. The prosthetic teeth projecting from the base are designed to look and function just like your natural teeth. Dentures are held in place primarily by the suctioning effect of their close fit against the alveolar ridges — that's why it's so important that they are fitted properly. The upper denture also gets extra support from the large surface area of the roof of the mouth (palate), which generally makes it extremely stable.
At first, wearing dentures may require some getting used to in terms of talking and eating, as the dentures become "balanced" in the space formerly occupied by the teeth. But over time, the muscles, nerves and ligaments of the mouth learn to work in new ways, which allows these functions to occur normally. Dentures also help support the facial skeleton and the soft tissues of the lips and cheeks, which can help create a more youthful appearance.
Types of Full Dentures
 Immediate Dentures: These are usually a temporary means of helping you transition to successful denture wearing. Because of the muscular readjustment required, as well as the natural shrinkage of gums, the dentures which are placed immediately after tooth extraction won't fit as well as permanent dentures made when the healing is complete. They do, however, provide you with new teeth right away, and give you time to adjust.
Immediate Dentures: These are usually a temporary means of helping you transition to successful denture wearing. Because of the muscular readjustment required, as well as the natural shrinkage of gums, the dentures which are placed immediately after tooth extraction won't fit as well as permanent dentures made when the healing is complete. They do, however, provide you with new teeth right away, and give you time to adjust.
Conventional Full Dentures: After a period of time, we can fabricate permanent dentures that conform to your mouth with near-perfect accuracy. These are carefully crafted to look as much like your own natural teeth as possible, and are able to function properly in your mouth for a long time.
Implant-Supported Overdentures: To increase the stability of a lower or upper denture, it's possible for it to be securely anchored using two or more dental implants. The upper jaw requires more implants (generally three or more) than the lower jaw due to a lesser bone density. Many people find this option offers a great balance of comfort, functionality and value.
Types of Partial Dentures
Transitional Partial Dentures: These relatively inexpensive removable plastic dentures serve as a temporary tooth replacement and space maintainer as you wait for your mouth to heal from tooth extraction, for example. Once the healing process is complete, dental implants can be placed.
Removable Partial Dentures (RPDs): Usually made of cast vitallium, these well-constructed, metal-based removable partial dentures are much lighter and less obtrusive than those made of plastic. They are a little more expensive than plastic dentures but will fit better. They are, however, much less expensive than implants or fixed bridgework.
How Dentures Are Made and Fitted
 Making quality dentures is a blend of science and art. First, an accurate impression (mold) is made of the alveolar ridges on the top and bottom of your mouth. The base of the denture is made from this mold in a dental laboratory. Working together, the dentist and lab technician choose from among many different sizes and shapes of prosthetic teeth to re-create a natural-looking smile. When everyone is satisfied with the result, the temporary dentures are made in permanent form.
Making quality dentures is a blend of science and art. First, an accurate impression (mold) is made of the alveolar ridges on the top and bottom of your mouth. The base of the denture is made from this mold in a dental laboratory. Working together, the dentist and lab technician choose from among many different sizes and shapes of prosthetic teeth to re-create a natural-looking smile. When everyone is satisfied with the result, the temporary dentures are made in permanent form.
To enable normal speech and eating, it's crucial to balance your bite. This means that the upper and lower dentures come together and properly stabilize each other. We carefully check the form and function of the dentures to ensure that they are working and fitting properly.
What to Expect After You Get Dentures
If you've recently lost your teeth and received an immediate denture, it's normal to find some tissue shrinkage and bone loss occurring. Therefore, in several months you may find that your immediate dentures no longer fit well. You will have two choices at this point: You can have your immediate (temporary) dentures re-lined. This means that material is added under the denture's base to better conform to the new contours of your alveolar ridge. A better option is to move to a set of conventional full dentures, which will last longer and fit better. With proper care, dentures offer a functional, aesthetic and economical solution to the problem of tooth loss.
Tooth Extractions
Primary vs. Permanent Tooth Removal
 Generally the primary or "baby" teeth become loose on their own and the child can wiggle them out. Occasionally, a primary tooth may not become loose on its own and may block the eruption of its permanent replacement tooth. Roots on a primary tooth are generally smaller than their permanent tooth counterparts. Most children and adults who have a primary tooth removed have a very quick recovery time.
Generally the primary or "baby" teeth become loose on their own and the child can wiggle them out. Occasionally, a primary tooth may not become loose on its own and may block the eruption of its permanent replacement tooth. Roots on a primary tooth are generally smaller than their permanent tooth counterparts. Most children and adults who have a primary tooth removed have a very quick recovery time.
In the absence of periodontal disease or trauma, permanent teeth do not usually become loose on their own. Removal of a permanent tooth will require some modifications of your daily routine. In some situations, it may be best if you do not return to work after having a permanent tooth removed. We will give you written post-operative instructions to take home if you have a tooth removed in our office.
At your orthodontist's request or Dr. Steckelberg's diagnosis, primary and/or permanent teeth may be removed in our office to allow for an improved orthodontic result. This is done with careful consideration of the individual variables present.
Surgical Removal of Tooth
Sometimes a tooth is not able to be removed without creating a small surgical opening around that tooth. That extra opening can allow for better visualization, as well as removal of any bone that might be trapping your tooth in place. If your tooth requires surgical removal, you may need sutures, or "stitches." Dependent on the suture material used, you will usually need to return for a quick visit to have your sutures removed one week after your surgery.
We try to let you know before your appointment if surgical removal of your tooth is anticipated. However, some situations do arise that may necessitate a surgical opening. It is just important to keep in mind that removal of any tooth may require an additional follow-up visit in our office.
Wisdom Tooth Removal
If appropriate, Dr. Steckelberg does remove some wisdom teeth in our office. A current panoramic X-ray must be utilized in determining if you will need to have an oral surgeon remove your wisdom teeth.
Patients on Anti-Coagulant Treatment
If you are taking Coumadin, Warfarin, daily aspirin, or any other type of "blood thinner," modification may be needed prior to removing a tooth. Make sure to tell us if you are taking one of the newer anti-coagulant medications such as Pradaxa, Eliquis, or Xarelto, which are referred to as "blood slickers". Please make sure to let us know if you are on these medications, so that we can treat you properly. A consultation with your physician, as well as pre-operative blood tests, may be needed to determine the appropriate time for surgery.
Patients on Bisphosphonates
If you are taking medications from the bisphosphonate drug family, surgical dental treatment may be modified. Examples of these medications are: Actonel (risedronate), Aredia (pamidronate), Boniva (ibandronate), Didronel (etidronate), Fosamax (alendronate), Fosamax Plus D (alendronate), Skelid (tiludronate), and Zometa (zolendronic acid). Medications generally have two names: a brand name and generic name; we have listed the generic name in parentheses. Emerging research suggests increased caution be used before any dental surgical procedure is performed. Research is still in the early stages, but our office is striving to stay on top of this recent discovery.
The concern about bisphosphonate emerged due to osteonecrosis of the jaw developing in patients who had invasive dental surgeries performed. The risk of developing osteonecrosis appears to be low, but we need to inform you of the risks and benefits, as well as any alternatives for any surgical procedures before the procedure is started.
You can learn more about osteonecrosis and other dental health topics at the American Dental Association website.
Wisdom Tooth Extraction
 In most people, the third set of molars, generally called "wisdom teeth," start coming in around age 17-25. However, the arrival of these teeth is often far from trouble-free. The extraction (removal) of one or more third molars is a relatively common procedure, performed on some 5 million patients every year. After a thorough examination and diagnostic tests such as x-rays or a CT scan, we may recommend that you have your wisdom teeth extracted. Here are some typical reasons why:
In most people, the third set of molars, generally called "wisdom teeth," start coming in around age 17-25. However, the arrival of these teeth is often far from trouble-free. The extraction (removal) of one or more third molars is a relatively common procedure, performed on some 5 million patients every year. After a thorough examination and diagnostic tests such as x-rays or a CT scan, we may recommend that you have your wisdom teeth extracted. Here are some typical reasons why:
- Your jaw may be too small to accommodate all your teeth, leading to excessive crowding and the chance of your wisdom teeth becoming impacted — that is, unable to emerge from the gums, and potentially harmful to adjacent bone or teeth
- Your wisdom teeth may be erupting (coming in) in a crooked orientation, which can damage other teeth or anatomical structures in the jaw, and/or cause bite problems
- If your wisdom tooth does not fully erupt (emerge from the gums), it can increase the chance for bacterial infection
- A cyst (a closed, fluid-filled sac) may develop around the unerupted wisdom tooth, which can cause infection and injury to the adjacent bone or nerve tissue
Whether it is aimed at preventing future problems or needed to alleviate a condition you already have, the extraction of wisdom teeth can be an effective treatment. But, as with all medical procedures, its benefits must be weighed against the small risk of complications. We will be happy to discuss in detail all the risks, benefits and alternatives in your individual case.
The Extraction Procedure
 Wisdom tooth extraction is usually an in-office procedure which may be performed by a dentist or an oral surgeon. It's quite possible to have the treatment done with only a local anesthetic (numbing shot) to keep you from experiencing any pain; however, if multiple teeth are being extracted at one time (as is often the case), a general anesthetic or conscious sedation may be administered. We will talk to you beforehand about the type of anesthesia that's best for you.
Wisdom tooth extraction is usually an in-office procedure which may be performed by a dentist or an oral surgeon. It's quite possible to have the treatment done with only a local anesthetic (numbing shot) to keep you from experiencing any pain; however, if multiple teeth are being extracted at one time (as is often the case), a general anesthetic or conscious sedation may be administered. We will talk to you beforehand about the type of anesthesia that's best for you.
Once you have been appropriately anesthetized, the gum tissue at the extraction site may need to be opened if the tooth is impacted. The tooth itself will then be gently removed. When the extraction is complete, you may need to have the site sutured (stitched) to aid healing. After the procedure is over, you will rest for a short time before going home. Depending on what type of anesthesia you have had, you may need another person to drive.
After the Procedure
The recovery period after wisdom tooth extraction generally lasts only a few days. During this time, you should rest when possible to encourage healing, and take any pain medication as prescribed. It's normal to experience some bleeding at the extraction site; this can be controlled by gently biting on gauze pads, changing them as needed, and resting with the head elevated on pillows rather than flat.
Holding an ice pack on the outside of your cheek for a few minutes at a time (for example, 5 minutes on / 5 minutes off) may help reduce swelling on the first day after the procedure. Starting on day 2, the warm moist heat of a washcloth placed on the cheek may make you more comfortable. Rinsing the mouth with warm salt water a few times a day can also help relieve discomfort.
You may want to eat soft foods for a few days after the extraction; likewise, be careful when brushing or putting anything in your mouth until your healing is complete. Be sure to follow the post operative instructions we will give you, as each situation is a little different, and we want you be as comfortable as possible.
Root Canals
Root Canal Treatment or Endodontic Therapy

A "root canal" procedure involves accessing the middle or core of the tooth. An opening is made in the chewing surface of the infected tooth. Through this opening, the nerve and blood vessels are removed and the open space, or canal, is cleaned and shaped. A special filling material called gutta percha, is placed in the canal to seal the tooth and prevent further infection. A regular filling material, either amalgam or composite, is then placed in that opening of the chewing surface of the tooth. Most teeth that have had endodontic therapy will require the additional support of a crown.
Root canal therapy may be indicated in the following situations:
- deep dental decay that has reached the tooth's nerve
- traumatic injury to face and teeth
- to allow for a post to help restore a fractured tooth
- to remove inflammation to reduce severe tooth sensitivity
- to provide more space to cover a poorly shaped tooth
Teeth that need endodontic treatment and have complicated anatomy, difficult access, or unusual presentation are typically referred to a specialized dentist, called an endodontist. We are fortunate to have more than one endodontist available in Lincoln. An endodontist performs root canal treatment and then you return to our office for the final restoration of that tooth. Dr. Steckelberg will build up the missing tooth structure and usually place a crown over that tooth to protect it from possible fracture. Sometimes a post may also be placed into the root canal filling material for added support.
Root Canal Retreatment
Not all teeth respond properly to non-surgical endodontic treatment. These teeth will be referred to an endodontist for evaluation and further treatment, if indicated. With modern advances in dentistry, we are able to save more teeth than our predecessors in the dental field. In endodontic retreatment, often the root canal is re-opened and retreated non-surgically.
Sometimes, a surgical procedure called an apicoectomy may also be performed. This involves removing residual infection present at the root tips and is done by a dentist specially trained in this procedure.
Our office may collaborate with an endodontist and a periodontist if you have a complicated dental situation. Occasionally, a tooth may not be able to be saved and will need to be removed, or extracted. We are able to remove most teeth in our office.
Dental X-Rays
Amount of Radiation

Did you know that everyone is exposed to radiation in our everyday lives? The amount of radiation you are exposed to with 4 bitewings or a Full Mouth Series of X-rays is less than the amount of average radiation in the U.S. from natural sources.
At Steckelberg Dental, we utilize the American Dental Association's guidelines for prescribing dental radiographs, including the ALARA principle. The ALARA principle means taking X-rays at ‘As Low As Reasonably Achievable' amounts of radiation exposure. More information can be found at the American Dental Association website.
Types of X-rays
- 4 Bitewings. These X-rays examine in-between your back teeth only. They will show bone height around your teeth, as well as cavities between your teeth. It is common to have these X-rays taken on a regular basis, as they show problem areas that are very difficult for your dentist to visualize or feel until the problem is large. Our goal as dental providers is to diagnose dental problems in the earliest stage possible.
- Periapical X-ray. A periapical X-ray typically shows the complete tooth structure, including crown and complete root of one to two teeth. We will often abbreviate this X-ray as a PA. It is common to have this X-ray taken if you are having a toothache or if dental infection is suspected.
- Panoramic X-ray. A panoramic X-ray (or "Pano") shows all your teeth, your temporomandibular joint, part of your maxillary sinuses, and both your jaw bones. It is useful in determining the location and number of permanent teeth present in a child. A Pano is also routinely taken every 5-7 years as a general survey of your oral anatomy and if wisdom teeth removal is indicated. It is important that our office has a copy of a recent Pano or Full Mouth Series on file for each patient to compare if problems arise.
- Full Mouth Series. A Full Mouth Series (FMS) is a set of 14-18 individual X-rays, typically including 4 bitewings and 14 periapical X-rays. If you have had much dental treatment in the past, this may be the general survey taken of your mouth every 5-7 years. Insurance will typically cover either a Pano or FMS every 3-5 years.
- Occlusal X-rays. Two occlusal X-rays are usually taken at the first opportunity available during your child's visit to our dental office. These special X-rays allow early intervention for dental problems including: extra teeth, missing permanent front teeth, cysts, abscesses, growths, and a cleft in the roof of the mouth (cleft palate). With the exception of traumatic injury, occlusal X-rays are usually only taken once during a patient's lifetime.
Frequency of X-rays
Dr. Steckelberg determines how often you should have dental X-rays based on your individual needs. If you are a patient that has experienced a large amount of dental decay, then we will recommend that you have dental X-rays more often than a patient who has never had a cavity.
Decision to take a dental X-ray is also based on your current situation. If you are experiencing dental pain, X-rays may also be necessary.
You have the option to refuse dental X-rays. You will need to sign an entry in your chart indicating that you have decided against the recommended X-rays. Unfortunately, x-rays are necessary for the diagnosis of many dental problems. If we have a concern about your choice, we will inform you of the risks you may face with your decision.
